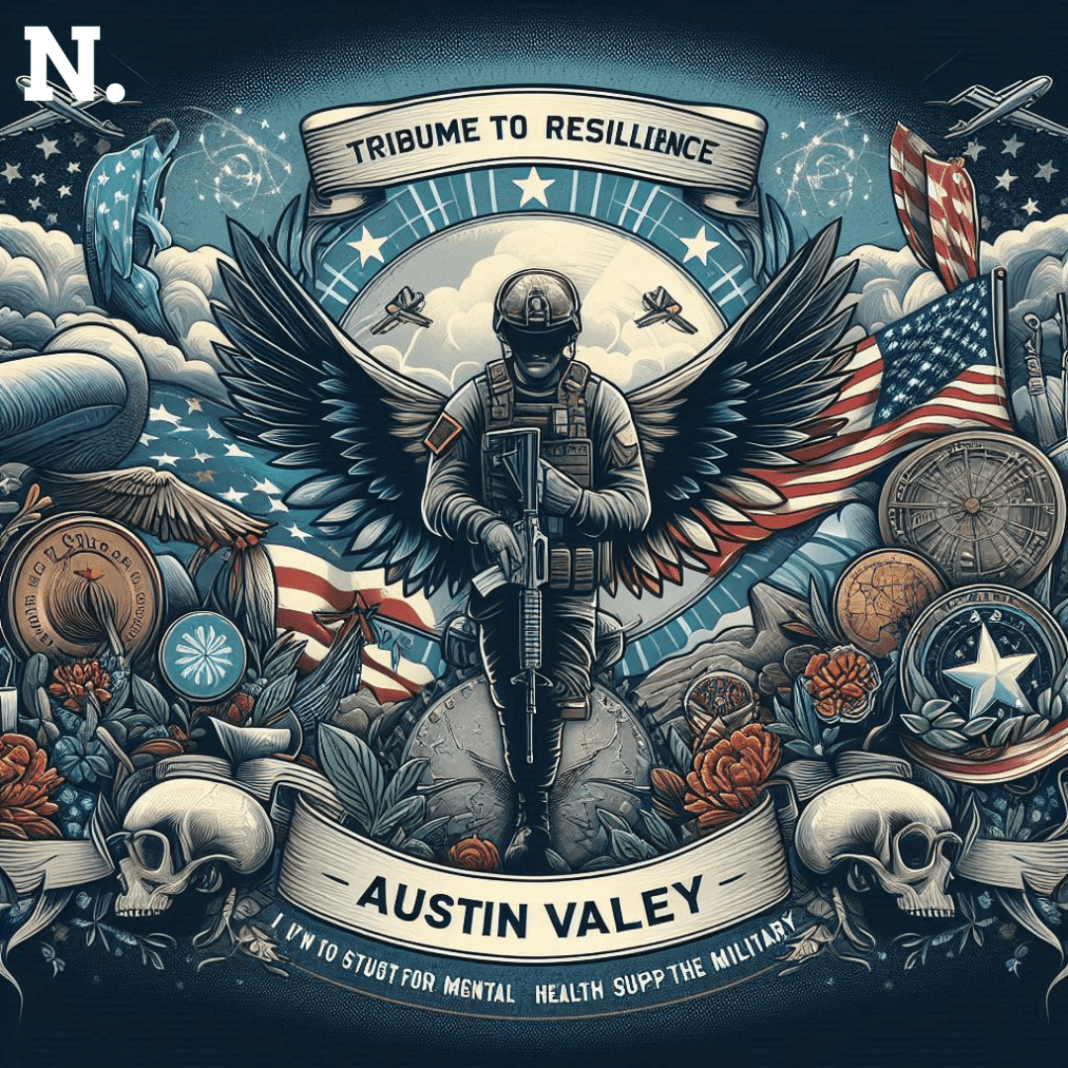
The tragic death of young and promising soldier Austin Valley has again brought to harsh light a deepening crisis within the U.S. Army: the alarming rate of suicides among soldiers even in peacetime. Valley’s death serves as a grim reminder of the mental health challenges faced by service members, raising urgent questions over the support system in place to cope up with these issues.
Valley Death Highlights: A Rising Epidemic
Only 23, Valley would take his own life on June 15, the event sending shockwaves throughout Fort Bragg and the broader military community. His death marks the latest in a heartbreaking trend: the Army struggles to cope with an explosion in suicides that has endured despite a deluge of prevention programs. According to the Department of Defense, the suicide rate has increased by 20% among active-duty soldiers over the last five years—with a most recent spike during the COVID-19 pandemic.
Austin Valley: Untold Story
The story of Austin Valley, however, is particularly gut-wrenching. By the Books,Valley, a good serviceman, was renowned for his leadership skills and bonhomie. Colleagues regarded him as a symbol of hope and strength. But, like many soldiers, he silently fought his personal terrors—the mental and emotional cost of military life. Friends and family describe him as a “pillar of strength” who, unbeknownst to many, bore the weight of invisible wounds.
“I knew Austin as a strong, capable, and motivated individual,” said Staff Sergeant John Lewis. He was very close to Valley; in fact, he had been his friend and mentor. “His death is a stark reminder that no one is immune to mental health struggles, no matter how resilient they may seem from the outside looking in.”
The Silent Battle
The terrible incident has brought into sharp relief the Army’s inadequate mental health support. The Army’s “Ready and Resilient” campaign has not been efficient in this regard so far, notwithstanding there are claims for it to be effective. Even an increased level of sophisticated mental health screening still cannot break through the stigma that remains the real obstacle to seeking help.
“Dr. Lisa Turner states that soldiers often view admitting to mental health issues as a sign of weakness that could harm their careers, causing many of them to believe otherwise,”. A clinical psychologist who has worked heavily in military mental health. The stigma and strong pressures of military life combine to create mental health crisis situations.
Institutional Response end
With this crisis, the Army has begun a host of programs to decrease stigma and increase mental health support. Programs range from confidential counseling services to peer support networks and training, to help soldiers recognize and respond to signs of distress among their fellow peers.
First and foremost, Lieutenant General James Richardson, deputy chief of staff for Army Personnel, called for a culture change within the military: “We must ensure that requesting help is viewed as a sign of strength and not as a weakness. Our soldiers are our greatest resource, and their mental health is as important as their physical readiness.”
Leader’s Role
Effective leadership is instrumental in combating the current suicide crisis. Commanders and senior leaders are learning how to open their doors to discussion and to promote supportive climates within their units; recognizing indications of mental distress, encouraging soldiers to avail themselves of resources without fear of retribution or negative career impact.
“We’ve got to set the example,” said Major General Mark Simmons, commanding officer at Fort Bragg. We can be more supportive and resilient by openly talking about mental health issues and taking care of our soldiers’ welfare when they are raised.
A Call for Comprehensive Solutions
While clearly steps in the right direction, a more comprehensive solution is needed to increase the availability of mental health professionals and reduce administrative and operational barriers to taking care. It also calls for culturally-appropriate mental health resources targeted at certain soldier issues.
“The complexity of military life requires a multifaceted approach to mental health,” Dr. Turner said. “It’s not about just providing services, it’s about setting up a culture that values mental well-being from top to bottom.”
Austin Valley’s death is a grim reminder of an ongoing suicide crisis within the Army but also acts as a catalyst for change. There is now a revamping of the pledge to tackle the deeper issues at play in this epidemic, as the military community comes to terms with this loss.
With its culture of openness, comprehensive support, and priority given to mental health initiatives, the Army can ensure that no soldier meets an end like Valley’s.
In the wake of this tragedy, it is very evident that the Army’s most vital battle lies not on foreign soil but within its own ranks. The challenge now before them is making sure that no soldier will ever bear his struggle alone and that help is always within reach.